Adult Medical Day Care Providers Improperly Billed NJ Medicaid
Table of Contents
- Posted on - 10/31/2023
- Introduction
- Background
- Methodology
- Findings
- Discussion of DMAHS and MCO Comments
- Conclusion
- Recommendations
Introduction
The Office of the State Comptroller, Medicaid Fraud Division (OSC) conducted this review to identify adult medical day care (AMDC) providers who improperly billed the Medicaid program for duplicative services or who billed for services that exceeded the amount the program permits to be billed. AMDCs are facilities that provide ambulatory care services to adults who require assistance with activities of daily living, including bathing, mobility, and eating. These medically necessary services enable individuals to continue living in a community setting.[1]
Through this review, OSC identified 21 AMDCs that violated Medicaid regulations by (1) impermissibly billing for more than five days in a week;[2] (2) billing for services to a beneficiary while that beneficiary was actually in an inpatient facility such as a hospital;[3] and (3) billing for services provided to a beneficiary when in fact another AMDC also billed for the same services to the same beneficiary on the same date.[4] As a result of this review, OSC identified approximately $946,087 in improperly spent Medicaid funds, and thus far, has recovered $839,000 of that amount.
These problems show a pattern of improper billing by AMDCs that could range from careless mistakes to fraudulent billing errors. These errors also have potential implications for the quality of care provided by the AMDC. If an AMDC cannot keep accurate records showing when a beneficiary is present at the facility versus in the hospital, there is a higher risk that the facility may not know what services need to be performed for a beneficiary or whether a beneficiary has received medically necessary services. Proper record-keeping helps ensure both that the Medicaid program is not overpaying for services but also that beneficiaries are receiving the care that they need.
There is more work to do in this area, and OSC has identified dozens of additional AMDCs that billed and received Medicaid overpayments for these same types of improper claims. OSC recommends systemic fixes to address the problems identified above and will continue to pursue recoveries for these improperly spent Medicaid funds.
Background
OSC is an independent agency responsible for monitoring and auditing government programs and agencies, reviewing the efficiency and effectiveness of government functions and programs, identifying cost savings, preventing misconduct within the programs and operations of government agencies, and investigating fraud, waste, and abuse. The State Comptroller is charged with implementing the Medicaid Program Integrity and Protection Act, N.J.S.A. 30:4D-53 to -64, by, among other things, ensuring that the State spends its Medicaid resources in a responsible and effective manner. OSC performs these duties through its Medicaid Fraud Division.
Medicaid is a joint federal and state program administered by states.[5] In New Jersey, the Division of Medical Assistance and Health Services (DMAHS) within the Department of Human Services administers the Medicaid program.[6] DMAHS, both directly and through its contracts with five managed care organizations (MCOs),[7] administers health coverage for over two million residents, including residents who are aged, blind, disabled, and earn low to moderate incomes.[8]
AMDCs provide ambulatory care services to adults who require assistance with activities of daily living, including bathing, mobility, and eating.[9] These medically necessary services enable individuals to continue living in a community setting. In order to participate in the Medicaid program, AMDCs must be licensed by the Department of Health and must agree to abide by all Medicaid requirements, including requirements regarding documentation.[10] The beneficiaries that AMDCs service must be clinically eligible to receive these services, and the AMDC must provide a minimum of five hours of services per day, with a maximum of five days of services provided per week.[11] AMDC services shall not be duplicative of services that the individual is already receiving, such as inpatient care at a facility and/or services at another AMDC.[12] In order to receive payment from the Medicaid program, AMDCs must agree to accept the Medicaid fee schedule, a per diem rate, and further agree to follow all Medicaid rules, including the five day per week service limit.[13] The program defines a week as seven calendar days, Sunday through Saturday.[14] Beneficiaries may elect to transfer services from one AMDC to another. If they wish to do so, they must request the transfer in writing, including the reason for the change. Transfers from one AMDC to another are reviewed and approved by the Division of Aging Services within the Department of Human Services.[15]
Methodology
For Medicaid dates of service ranging from January 1, 2016 through May 31, 2022 (“review period”), OSC identified AMDCs that billed for services improperly under the following three scenarios:
- AMDC billed for services provided to beneficiaries who were also inpatient at a facility (in violation of N.J.A.C. 10:164-1.5(g)(3));
- AMDC billed in excess of five days of service in a week for an individual beneficiary (in violation of N.J.A.C. 10:164-1.6(i)); and
- AMDC billed for services for the same day, same service, and same beneficiary as another AMDC provider (in violation of N.J.A.C. 10:49-9.8 and N.J.A.C. 10:164-1.5(g)(1)).
OSC identified the providers that received the highest overpayment amounts for these three scenarios (combined), sent notices to each party explaining the findings, and afforded each AMDC ample opportunity to provide information to rebut OSC’s findings. Some AMDCs agreed to the initial findings and paid the identified amount in full. Others provided rebuttal information, which OSC considered and, as appropriate, adjusted its findings accordingly. All overpayment amounts referenced below take into account these adjustments. In total, OSC issued notices to the following 21 AMDCs, with the outcome for each noted below.
Chart 1: 21 AMDCs with the Highest Total Overpayment Amounts[16]
|
AMDC Name |
County |
Total Overpayment |
Status |
|
New Life Adult Day Care |
Bergen |
$173,461.90 |
Paid in Full |
|
Peaceful Adult Day Care |
Bergen |
$130,141.60 |
Paid in Full |
|
Golden Path Adult Day Care |
Middlesex |
$126,782.20 |
Paid in Full |
|
Signature Medical Day Care |
Essex |
$79, 079.00 |
Paid in Full |
|
Atmiya Adult Day Care |
Bergen |
$60,367.80 |
Paid in Full |
|
Fivestar Adult Medical Day Care |
Union |
$52,115.30 |
Paid in Full |
|
2nd Home Union City Operations, LLC |
Hudson |
$43,905.10 |
Agreed to Pay in Full |
|
Home Away from Home Adult Day Care Center of Nutley Home Away from Home Adult Day Care Center of Nutley Settlement Agreement |
Essex |
$43,356.20 |
Paid in Full |
|
Town Square Medical Day Care |
Union |
$36,956.00 |
Paid in Full |
|
Jersey Shore Medical Day Care |
Monmouth |
$29,350.33 |
Paid in Full |
|
Xanadu Adult Medical Day Care |
Passaic |
$24,385.10 |
Non-Responsive |
|
Alliance Adult Medical Day Care Services, LLC Alliance Adult Medical Day Care Services, LLC Settlement Agreement |
Camden |
$21,409.40 |
Paid in Full |
|
Golden Years Adult Day Care Center, LLC Golden Years Adult Day Care Center, LLC Revised Notice of Overpayment |
Passaic |
$20,247.40 |
Paid in Full |
|
The Care Factory, Inc. |
Passaic |
$17,597.20 |
Paid in Full |
|
2nd Home Newark Operations, LLC |
Essex |
$15,584.40 |
Agreed to Pay in Full |
|
Sunshine Adult Day Health Care Center |
Bergen |
$14,573.70
|
Paid in Full |
|
Mi Casa Es Su Casa II, Inc. |
Hudson |
$14,031.70 |
Non-Responsive |
|
South Amboy Adult Day Healthcare Center South Amboy Adult Day Healthcare Center Revised Notice of Overpayment |
Middlesex |
$12,283.10 |
Paid in Full |
|
Rainbow Home Medical Day Care |
Somerset |
$12,050.10 |
Paid in Full |
|
Stars Adult Medical Day Care Center |
Camden |
$9,235.60 |
Paid in Full |
|
2nd Home Sweet Home Operations, LLC |
Union |
$9,173.60 |
Agreed to Pay in Full |
|
|
TOTAL |
$946,086.73 |
|
Findings
A. AMDCs Billed Medicaid Even Though the Beneficiary Was in an Inpatient Facility
OSC found that, during the review period, the 21 AMDCs listed above billed and were erroneously paid by the Medicaid program for 2,337 claims, totaling $192,612, while these beneficiaries were receiving inpatient services in another facility (in violation of N.J.A.C. 10:164-1.5). In essence, this means that Medicaid was billed twice – for day care services and inpatient services – when the Medicaid beneficiary was only receiving services at the inpatient program. The AMDCs were being paid for services they did not deliver—resulting in a waste of taxpayer funds.
Below is a chart showing the top 5 AMDCs, out of the 21 under review, with the highest overpayment amounts under this scenario.
Chart 2: Top 5 AMDCs with Highest Overpayment for Services for Billing Medicaid When the Beneficiary Was Inpatient in a Facility[17]
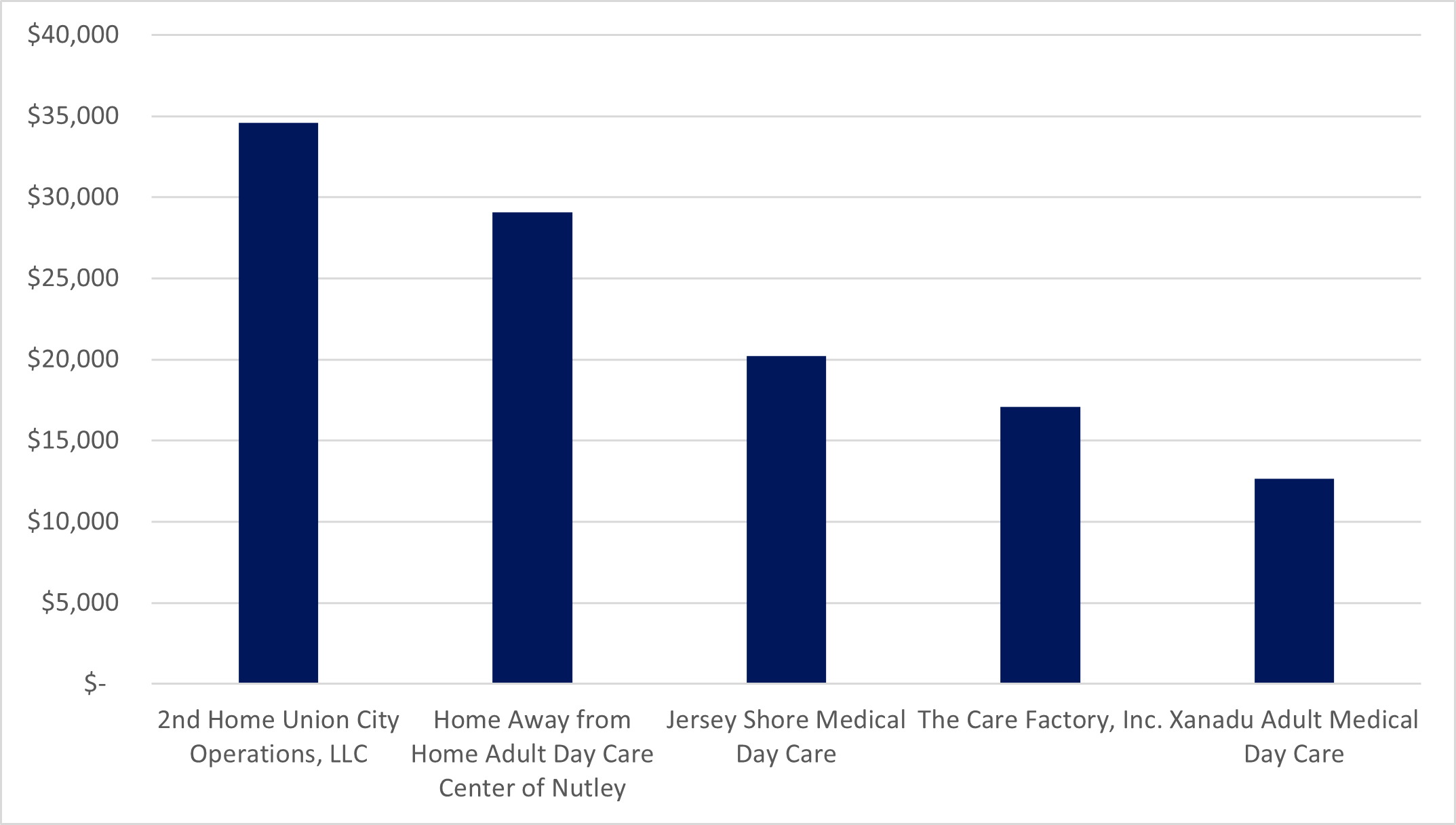
Some AMDCs provided documentation in response to this finding, such as sign-in sheets showing that a beneficiary was on site at the AMDC, and OSC revised its findings accordingly. Other AMDCs, however, did not provide any documentation to rebut or otherwise explain why they billed for providing services to a beneficiary who was inpatient at a hospital or other facility, and OSC maintained its initial findings for those AMDCs.
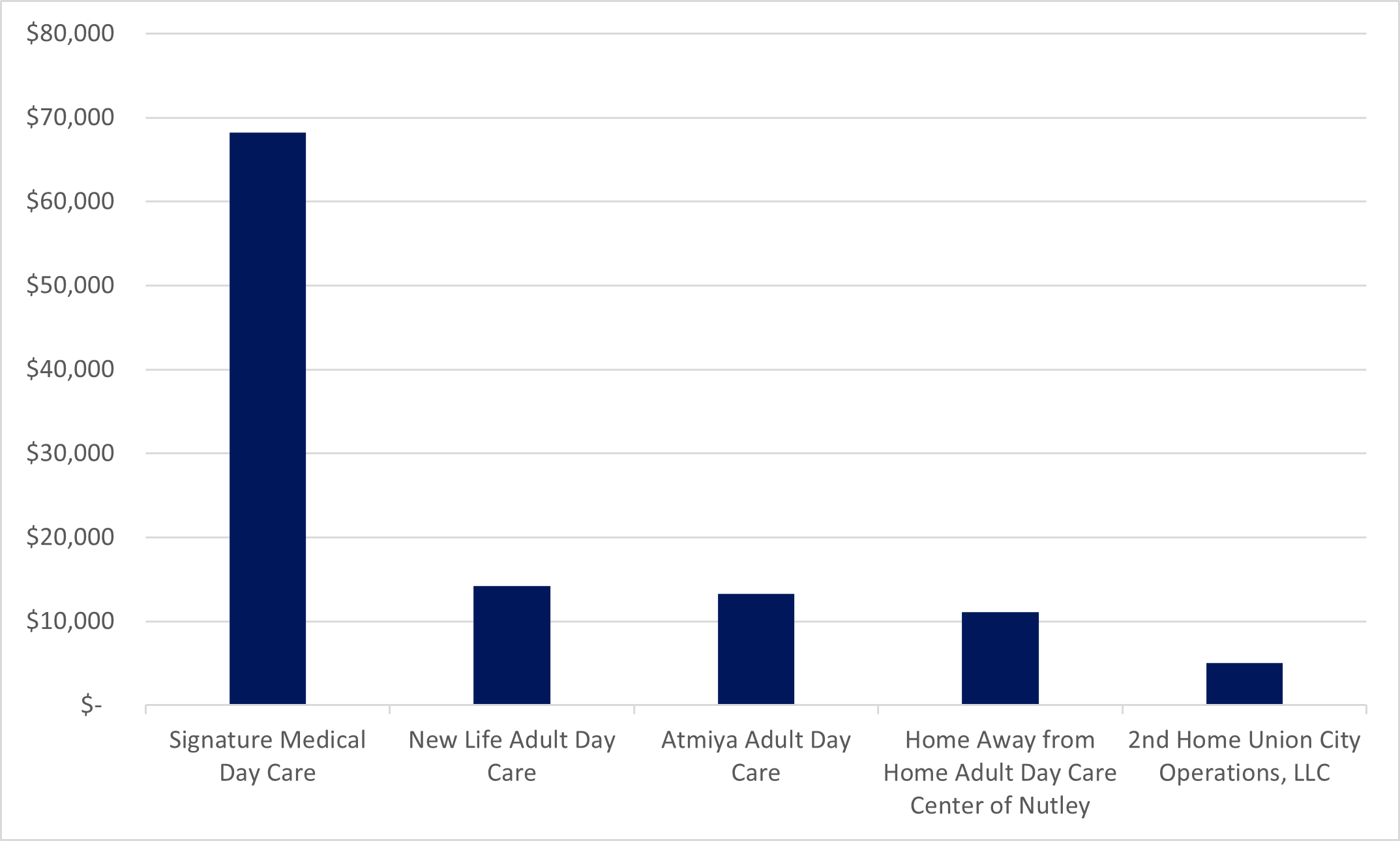
B. AMDCs Improperly Billed for Services in Excess of Five Days a Week
During the period of review, the 21 AMDCs listed above improperly billed and were paid by the Medicaid program for 7,849 claims, totaling $613,286 in which the AMDC billed in excess of five days of service per week for an individual beneficiary. This violates N.J.A.C. 10:164-1.6, which prohibits providers from billing for more than five days per week. This was the most common and most costly issue identified in OSC’s review.
Below is a chart showing the top 5 AMDCs, out of the 21 under review, with the highest overpayment amounts for this scenario.
Chart 3: Top 5 AMDCs with Highest Overpayment for Services in Excess of 5 Days

A number of the AMDCs under review claimed that their improper billing stemmed from changes in billing practices resulting from the public health emergency. None of the AMDCs, however, provided a substantive reason that would justify billing for services that were either not provided or not permissible.
C. AMDCs Billed Medicaid When Another AMDC Provided and Billed for Identical Services
During the review period, the 21 AMDCs listed above improperly billed the Medicaid program for 1,720 claims and the program paid these providers a total of $140,189 for services provided to a beneficiary for the same day, same service, and same beneficiary as another AMDC (in violation of N.J.A.C. 10:49-9.8 and N.J.A.C. 10:164-1.5(g)(1)). Again, this finding is problematic because it indicates that the Medicaid program was being double billed—billing for the same service allegedly provided by two different AMDCs to the same recipient on the same day.
Below is a chart showing the 5 AMDCs, out of the 21 under review, with the highest overpayment amounts for this scenario.
Chart 4: Top 5 AMDCs with Highest Overpayment for Services Billed and Provided by Another AMDC
If an AMDC submitted adequate documentation to rebut OSC’s initial findings, including sign-in sheets and/or telephone logs showing services were provided, OSC gave credit for such services. The above chart reflects the modified claims.
Discussion of DMAHS and MCO Comments
OSC provided a discussion draft of this report to DMAHS and the five MCOs for review and comment. DMAHS and four MCOs formally responded; one MCO acknowledged receipt of the report but did not submit formal comments. DMAHS and two of the MCOs agreed with the recommendations below. One MCO suggested that OSC address the problems outlined in the report by modifying the MCO Contract. Another MCO stated that requiring MCOs to deny improper claims would be “inequitable,” and it instead suggested that DMAHS and the MCOs pay these claims and then retroactively identify and recoup any overpayments. OSC disagrees with these suggestions because there is no need to modify the MCO Contract’s existing, easy-to-understand legal requirements. The MCO-proposed “pay and chase” approach is far less efficient and effective than the systemic approach that OSC recommends below.
Conclusion
The overpayments described above are almost entirely avoidable through two parallel processes. The AMDCs, for their part, should more carefully review their documentation prior to submitting claims for payment to ensure that they submit claims only for services provided and appropriately documented, and that do not exceed the five day per week limit. DMAHS and the MCOs, for their part, should implement claim processing/payment edits[18] or procedures to ensure that they do not make payments for duplicate claims or those that exceed the five day per week limit. These steps would result in savings of hundreds of thousands of dollars annually for the Medicaid program.
Recommendations
In view of the findings in this report, OSC makes the following recommendations:
- DMAHS and the MCOs should implement a claims edit to deny AMDC claims when an inpatient claim was already paid for the same beneficiary and date of service.
- DMAHS and the MCOs should implement a claims edit to deny any inpatient claims when AMDC services were already paid for the same beneficiary and date of service.
- DMAHS and the MCOs should implement a claims edit to deny AMDC claims in excess of five days in a week.
- DMAHS should require that AMDC providers and/or their billing companies put systems in place to ensure that they do not bill for claims in excess of five days in a week.
- DMAHS and the MCOs should implement a claims edit to deny AMDC claims when another AMDC claim was already paid for the same beneficiary and date of service.
- DMAHS should require that AMDC providers and/or their billing companies put systems in place, including maintenance of adequate documentation, to ensure that they do not improperly bill for claims for a beneficiary who is no longer receiving services at the AMDC and/or is receiving inpatient services.
Footnotes
[1] See N.J.A.C. 10:164 et seq.
[2] See N.J.A.C. 10:164-1.6(i).
[3] See N.J.A.C. 10:164-1.5(g)(3).
[4] See N.J.A.C. 10:49-9.8 and N.J.A.C. 10:164-1.5(g)(1).
[5] See https://www.hhs.gov/answers/medicare-and-medicaid/what-is-the-difference-between-medicare-medicaid/index.html.
[6] See https://www.nj.gov/humanservices/dmahs/home/about/.
[7] See https://www.nj.gov/humanservices/dmahs/info/resources/care/index.html.
[8] See https://njfamilycare.dhs.state.nj.us/analytics/home.html.
[9] See N.J.A.C. 10:164-1.1, 1.2, and 1.5.
[10] See N.J.A.C. 10:164-1.3.
[11] See N.J.A.C. 10:164-1.1, 1.4, 1.5, and 1.6.
[12] See N.J.A.C. 10:164-1.5(g).
[13] See N.J.A.C. 10:164-1.6.
[14] Pursuant to N.J.A.C. 10:164-1.6(i)(1), "week" means seven calendar days, starting on Sunday and continuing through Saturday.
[15] See N.J.A.C. 10:164-1.7.
[16] AMDCs with the status “Paid in Full” paid the full amount identified by OSC, either upon notice from OSC or by virtue of a Settlement Agreement reached with OSC. AMDCs with the status “Agreed to Pay in Full” are in the process of paying the Medicaid program the identified overpayment under a payment plan. AMDCs with the status “Non-Responsive” did not respond to OSC’s notices, and, as a result, OSC is withholding their current claims in order to collect the identified overpayments.
[17] Xanadu Adult Medical Day Care has been non-responsive.
[18] A claims processing edit is a cost-containment tool used to automatically identify, flag, or reject a particular claim that may be impermissible.

Press Contact
Pamela Kruger
Pamela.Kruger@osc.nj.gov
609-789-5094
Waste or Abuse
Report Fraud
Waste or Abuse
 Official Site of The State of New Jersey
Official Site of The State of New Jersey